Video tutorials to support ST2/3 trainees approaching final exams - The Home Help Series
News - updated 12/1/2021 (Vaccination, Additional work, Wellbeing, Consideration, Educational Development)
ARCP - updated 5/5/2020
AKT / CSA and the RCA (CSA temporary replacement) - updated 12th Aug 2020
Supervision
Support
Visas
Workplace Based Assessment Changes
Video tutorials to support ST2/3 trainees approaching final exams - The Home Help Series

Episode 1 - About the changes afoot
Episode 2 - How to record remote video consultations, gaining consent remotely
Episode 3 - Analysing consultations in preparation for the RCA
Episode 4 - The latest updates about RCA recording
Episode 5 - Analysing consultations for the RCA - management
ARCP
- ST2s and ST3s ARCP dates will be 12 months from your last ARCP and should be detailed on your previous ARCP and the portfolio.
- ST1s may not have been given an official date yet but they are usually in the last week of June and first 2 weeks of July.
- You need to arrange your ESR not more than 8 weeks prior to your ARCP date. Get planning now with you educational supervisors. Educational supervisors, please ensure that you have created a new review period for your trainee.
- ESRs are usually done face to face, however during the crisis using video chat is acceptable.
- Please make a note on the ESR of how the meeting occured.
- A new guide for ARCP process during covid was reelased on 31/3/2020 'Gold Guide Version 8'
- The number of assessment required for work place based assessment has been reduced by 50% during the Covid 19 pandemic
- Allowances will be made to ensure that disruptions to training whilst working flexibly to deliver care during the Covid 19 pandemic will not disadvantage trainees and their progression.
- End of training is considered to be the single critical progression point in GP
- Annual ARCP will continue but the panel can be reduced to 2 members (3 members for a 'non standard' outcome)
- ARCPs will now be held online with a panel chair and 2-3 panel members. There will be no lay representative or observers and no external RCGP asessor
- Online BLS certfiicates will be accepted during the Covid pandemic period due to lack of availablilty of face to face courses. The online certificate should mention automated external defibrillation (AED) OR the trainee shoujld add a reflective entry demonstrating an understanding of AED.
- A refelective learning log entry for child level 3 safeguarding is not required during the e Covid 19 pandemic.
- Adult safeguarding changes are not being implemented i.e. adult safeguarding certificates and reflective entries will not be required at present.
- CEPS (Cliinical Examination Procedures) - it may not be possible to demonstrate CEPS at present and therefore alternative evidence may be provided for those about to CCT. Acceptable are a CEPS reflective learning log entry and / or educational supervisor comments regarding competency in mandatory CEPS.
- Evidence numbers
-
| Item |
ST1 |
ST2 |
ST3 |
| CBD |
3 |
3 |
6 |
| COT/miniCEX |
3 |
3 |
6 |
| MSF |
1 or LLE |
- |
1 or LLE |
| PSQ |
waived |
waived |
waived |
| CSR |
1 per post |
1 per post |
1 per post |
| Logs |
As work permits |
As work permits |
As work permits |
| QIP/Audit |
waived |
waived |
waived |
| Form R |
required |
required |
required |
| BLS |
Online accepted |
Online accepted |
Online accepted |
| CEPS |
Some activity |
Some activity |
Mandatory CEPS |
| Sig Event |
1 for any event on form R |
1 for any event on form R |
1 for any event on form R |
| Safeguarding |
Online accepted |
Online accepted |
Online accepted |
AKT / CSA - and the RCA
Updated 23th June 2020
The Recorded Consultation Assessment will replace the CSA until further notice. The RCA will assess your ability to apply clinical, professional, communication and practical skills for general practice. You are being tested on the same competency and curriculum areas as tested by the CSA exam and to the same standard. i.e. can you practice safely and independently.
- 13 recorded consultations are to be submitted from your current working environment
- Consultations may be any combination of audio, video or face to face encounter and may include home working
- Details on the submission process is to be released and trainees closest to date of CCT are being prioritised
- For trainees sitting RCA before the 30th of September a fail at RCA will not be counted in your 4 allowed exam attempts to allow for the effect of disruption in training.
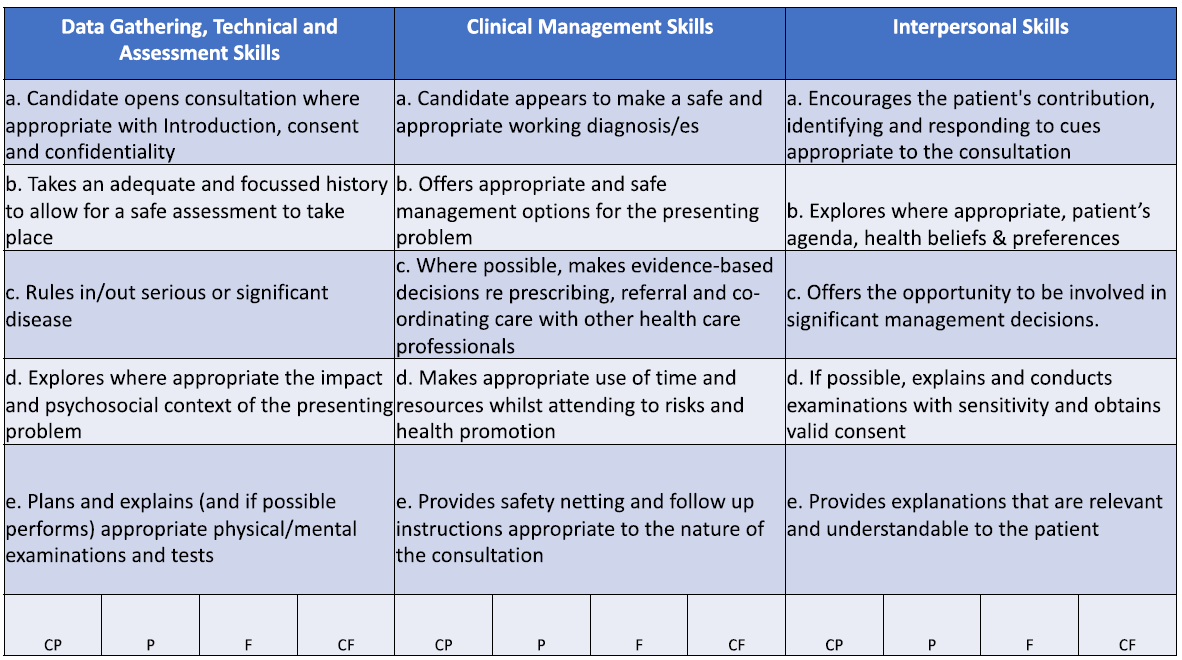
The RCA Marking Scheme
Top Tips for the RCA
1. Start early - start recording as soon as possible to get into the swing of it
2. Get the tech - speak to your trainers to make sure you have a webcam and are aware of the governance issues of recording and storing consultaitons
3. Get the right cases
- Cases submitted should be of an appropriate level of challenge sufficient to demonstrate safe and independent practice. See Appendix 1
- Pick cases that help you demonstrate their skills across a breadth of the curriculum
- Ensure there is sufficient evidence in all 3 domains for the assessment
- Reception/admin staff need to be ‘on board’ and know what is happening
- Engage reception/triage clinician to only book appropriate cases
- Simple triage consultations are unlikely to cover all three domains
- Agree with your practice to ‘be selfish’ and pick appropriate cases off other clinicians list
- Problems that are new are more likely to be suitable for submission
- Get other clinicians on board and involved with swapping of appropriate cases
- If individual GP surgeries offer pre-triage or electronic navigation prior to a consultation, ensure this isn’t detrimental to the consultation and use these systems to ensure appropriate case exposure
- If possible, only book willing/consenting patients to maximise opportunity.
- Make sure patients know that the call may come from a withheld or unrecognised number
- Be creative in how cases are identified – ask nurses for any newly diagnosed hypertensives / diabetics; following up on letters can sometimes work well
4. Balance workload with catch ups to get and stay in the right frame of mind for recording and to allow adequate time to review notes.
5. Keep up to date with the RCGP guidance which is updated regularly
6. A do not disturb sign on your door can help prevent interuptions during recordings
7. Use a desktop timer to help keep track of time
8. Consider prompt sheets to help you remember key consultation elements e.g. consent, identity checks, assessment of impact, ideas, concerns, expectations
9. Make notes as necessary but don't let note taking or typing distract from the flow of conversation
10. Reference any relevant medical history in the discussion. You should be asking contextually relevant questions but the examiner can't assess if questions are relevant if they don't have the context you therefore need to expose relevant history to the examiner by verbalising it.
11. Learn to assess the suitability of your consutlation against this grid:
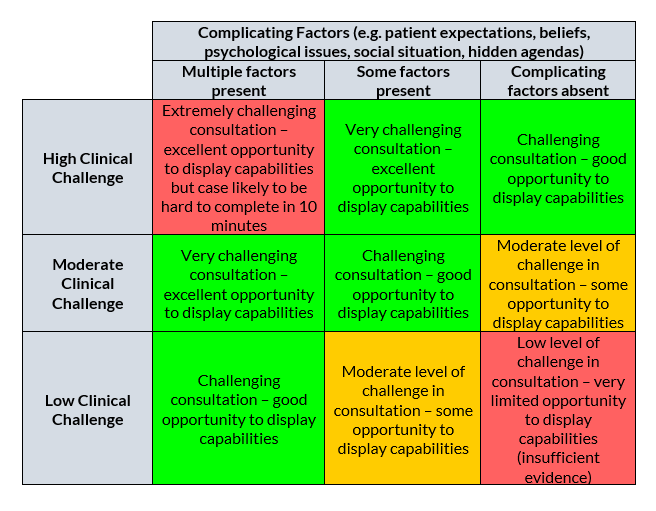
Cases which are of low clinical challenge will not provide sufficient opportunity for trainees to demonstrate capabilities.
Examples of cases of low clinical challenge:
- Follow up of well controlled chronic disease with minimal changes to current management
- Medication review with minimal changes to current management
- Low diagnostic challenge e.g. viral warts
- Health promotion consultation - limited opportunity to demonstrate data collection and diagnostic capabilities
- Appointments to request expedition of hospital appointemnts - limited oppotunity to demonstrate data collection and diagnostic capabilities
Video Tutorials for the RCA

Frequently Asked Questions
Supervision
- GP Trainees still need to be supervised at all times while they are working clinically.
- The supervisor for an individual session will often be the Educational or Clinical Supervisor themselves, but as before, this responsibility can be delegated by the ES/CS to another doctor in the training practice. If the trainee is working on another site, this should ideally be with their usual ES/CS. If this is not possible trainees should at all times be able to access a qualified GP (in person, or via telephone and/or video link) who is a trained clinical supervisor (ES/CS or OOH CS).
- Depending on the experience of the trainee, supervision can be either direct supervision (in the room), near supervision (in the building) or remote supervision (on the phone).
- The level of supervision required must be discussed with the trainee and should match their experience of working in that type of session. Trainees who can work under near supervision for face-to-face consulting may need direct supervision as they learn how to consult remotely. This may involve conducting some joint telephone surgeries until the trainee is ready to work under near supervision.
- Undertaking consultations with remote supervision should normally only be used for more experienced trainees. The trainee should agree that they are ready before moving to working under remote supervision. Trainees should not be lone working as the only doctor on site in a GP surgery, or in any alternative setting.
- The Covid-19 pandemic is throwing up some new contexts for supervision:
- Trainees working remotely due to self-isolation or shielding. Trainees undertaking telephone consulting or other remote clinical working (processing patient results, etc) should normally have contact with their supervisors at the beginning of each session (to confirm arrangements and check availability), and at the end for debriefing. A supervisor should be available at all times during the session to help them with queries.
- Trainees working in Covid-19 hubs will need appropriate induction and training before working in this environment.
- Trainees working in alternative settings. Sometimes, as a result of local service pressures, trainees will be pulled into working in training environments which are not currently GMC approved training sites. This is acceptable, but please follow the guidance in Appendix A
Appendix A
- In responding to the Covid-19 pandemic, the local healthcare system may require GPSTs currently based in GP practices to provide care in new and emerging community settings (e.g. Covid Response Hubs) or practices not currently approved as GP Training learning environments.
The nature of the pandemic and required response means flexibility and pragmatism are key, so such work should be facilitated where the following are taken into account.
• Prior to undertaking such work, GPSTs require the support and agreement of their Employer, Clinical and Educational Supervisors, and Primary Care Dean or nominated deputy
• All activities should be subject to the usual risk assessments of the service host including the provision of all necessary recommended equipment
• GPSTs should not work above their contracted hours without their and their employer’s agreement
• GPSTs shouldn’t work more than two sessions per week in this alternative setting, without the approval of the Primary Care Dean
• Wherever possible, trainees should work alongside one of their current supervisors
• There should still be protected time for breaks and rest in line with the Junior Doctors Contract
• Supervision is of vital importance. At all times, trainees should be able to access a qualified GP (in person, or via telephone and/or video link) who is a trained clinical supervisor
• A trained clinical supervisor is someone who is an existing GP or Foundation trainer, OOH GP training supervisor, or who can provide evidence of training in clinical supervision e.g. supervisor on the NHSE/PCN pharmacy programme
Support
- Formal Tutorial time and HDRC teaching have been suspended during the current pandemic. A full-time trainee can be based in the practice for 10 clinical sessions. Guidance is still in preparation on the current requirements for WPBA.
- However these 10 sessions should still normally include (inside the usual 40 hour working week) an opportunity for supervision and debriefing after each session with the supervisor for that session. The balance of clinical/admin time in each session should remain at 3:1, as before.
- Time should also be set aside each week (again, inside the 40 hour working week) for a fuller debriefing on the week with the supervisor. This should include discussion of challenging patients/scenarios and exploring the trainee’s responses to working in new ways and under an increased workload pressure.
- These 10 sessions should include the time that trainees need to spend in acquiring new knowledge and skills to practise safely during the Covid-19 pandemic, e.g. accessing telephone consulting training material.
- Local GP Programmes are organising virtual group work, using Skype or similar, usually on Tuesday or Thursday when the HDRC was running. Trainees tell us this is a really valuable opportunity for peer support, so supervisors should make every effort to release trainees for these times when clinical pressures allow.
- Support is still available to trainees in their local programme via their TPDs. HEE is also recruiting recently-retired GP educators to provide additional support in case TPDs need to devote more time to their clinical work as a result of workload pressures.
- If a trainee is struggling and needs additional support beyond what is immediately available then contact the programme Associate Dean for advice. The local HEE PSW team are also still available to provide additional support.
Visas
- Because of coronavirus (COVID-19), some NHS workers and their families will have their visas automatically extended for 1 year. To get the extension, you must:work for the NHS as a doctor, nurse or paramedic have a work visa that’s due to expire before 1 October 2020.
- The extension will apply from the date your visa is due to expire.
- UK Visas and Immigration (UKVI) will contact your employer to confirm your visa has been extended.
Workplace Based Assessment Changes

Guidance on the changes to workplace based assessment are shown here
News
08/01/2021
To all Associates in GP Training (GP Trainees) and Educational Supervisors
Vaccination Roll-Out and Additional Locum Shifts
We would like to thank you for all your hard work and dedication this year and for everything that you are doing to support our communities during the Covid pandemic. We appreciate that this has altered your training experience, and that primary care itself has changed dramatically. We will continue to support you, advocate for you and mitigate where we can but if you have specific concerns about your training progression please talk to your TPDs.
Covid activity levels across the country have risen sharply and within our region, several acute trusts are struggling with this dramatic increase. Primary care is also facing considerable challenges; we are aware that our GP trainees are integral to the sterling work being done within practices and the vaccination rollout is adding to the unprecedented challenges on an already stretched system.
Colleagues in Primary Care are offering to support the vaccination programme by undertaking sessions at Vaccination Centres or assisting the local efforts to vaccinate nursing homes and the housebound. Trainees can contribute to this effort either by undertaking GP surgeries freeing up other staff for the vaccination programme or by actively participating in vaccination clinics. It is thought that participation in 1-2 vaccination clinics would be a worthwhile educational and clinical activity. This can be undertaken during the clinical sessions of the working week. There may also be the possibility of additional vaccination sessions outside contracted hours which would have to be funded locally.
In several trusts within the West Midlands, Foundation Doctors have been moved for part of their GP attachments back to the Acute Trusts to support acute services within the hospital.
There are no current plans to move any trainees from General Practices.
GP Trainees within Acute Trusts may be asked to move into other departments such as Acute Medicine which are facing intense clinical pressure. These moves should be 1) approved by the Postgraduate Dean 2) should be fully supported and 3) for a finite length of time.
However, if any of you have additional experience or would like to undertake additional shifts to support the Acute Trusts then HEE would be supportive of this provided it was appropriate and sensible.
Any locum work within hospital or a vaccination/testing centre would be in addition to your standard working week and would take place with the following conditions:
Prior to Commencing any Additional Work:
- Trainees should be progressing as expected with their training. We would not want any additional work to interfere with that. The Educational Supervisor needs to be in agreement that current and future development is satisfactory and that additional shifts will not impact on educational progression.
- The current Clinical Supervisor needs to be in agreement with the additional locum work as this may impact on your current workplace and clinical responsibilities.
- The Lead Employer must be informed and in agreement. This is because they have Occupational Health responsibilities especially if any individual could be working in a high risk environment.
During any attachment:
- If you undertake additional hours in excess of the contacted 48hour week, you must notify the lead employer in order to sign a working time directive opt out form. This can be found in the most recent FAQs on the Lead Employer website.
- It is important that the requirements of the working time regulations are adhered to. This includes adequate rest breaks and provisions etc.
- There must be access to adequate personal protective equipment (PPE).
- All additional work must be under the supervision of a qualified clinical supervisor
- All doctors have a duty to recognise and work within their competence and particularly when working in an unfamiliar environment they must seek professional advice from appropriate colleagues.
- Any payments and related contractual arrangements for this additional work need to be negotiated directly with the CCG, practice or acute trust concerned.
- Additional locum shifts at an Acute Trust should ideally be undertaken where you have already worked so that you are familiar with their local processes
- The MDU has confirmed that you do not need any additional cover for such locum work.
- Trainees need to be mindful that additional employment will have implications for tax, NI and pension contributions and responsibility for these rests with the provider and the individual trainee.
- Any locum or other additional work must be declared on your Form R prior to your next ARCP.
Nationally, HEE is committed to supporting and protecting your training experience as much as possible during these incredibly difficult times and this is the approach we are continuing to follow.
We are very grateful for all your hard work in the very difficult circumstances of this pandemic. We would like to reiterate that the decision to undertake any additional work should be without duress and a personal decision for each trainee to make. In addition, there should be no ramifications for any trainee who declines to participate in any additional work for a Trust, Practice or local CCG.
We appreciate every trainee has very different circumstances and responsibilities and so any decision to undertake additional sessions must be a personal decision provided that ES, CS and Lead Employer are also in agreement. We would strongly encourage every doctor to ensure that they are vaccinated and would encourage any support for the vaccination programme whether by working back at the surgery or by actively participating in the vaccination process.
Wellbeing:
The GP School is very conscious that many of you are separated from family and friends living in other parts of the UK and internationally at a time when travel is extremely difficult. No matter who you are, it’s important to be conscious of your own mental health “barometer” and take positive action to reduce stress and improve general wellbeing. Please talk to someone if you are struggling (this could be your Clinical Supervisor, Educational Supervisor or Programme Director but there are also other sources of support available). The following link provides details of support from Lead Employer but also Practitioner Health and other support services.
https://sharedservices.sthk.nhs.uk/wp-content/uploads/2020/10/WellbeingResourcesDoc.pdf
The current focus for HEE and the GP School is trying to support trainees and trainers as much as possible without dropping standards. This means that trainees and trainers need to be working closely together and with each other. Neither should be making unreasonable demands on each other especially at a time when both groups are facing additional stresses of running surgeries of remote consultations, managing high risk individuals, working in systems under pressure and trying to support the massive vaccination programme.
There is a letter from HEE for trainees regarding GP Training and the Current Pressures attached to this current email.
Consideration:
We ask for on-going consideration of the stresses felt by trainee, trainer and also practice manager. It is important that appropriate respectful and professional behaviour shown by everyone. Trainees should be liaising with trainers about knowledge and evidence gaps of the eportfolio, log entries should be released in a timely way and trainers should be giving honest feedback on the evidence presented. In order to progress and develop in training and throughout a career, it is important to learn from both feedback and reflection.
Educational Development:
Looking forward, the GP School is in an amazingly strong position despite the pressures of last year. It is a credit to the programme directors and trainees that the move to remote education has happened so smoothly. A small minority of trainees have not engaged with remote learning which is worrying.
This is the equivalent of undertaking a University Degree without attending the lectures. There is no reliable alternative to getting through GP Training except by adopting the skills, behaviours and thinking behind being a GP.
This cannot be learnt from any single course but through the apprenticeship of being a GP within practice team as well as being an active part of a peer group within the GP Training Programme, supported and guided by the Programme Directors. We recognise that there are likely to be times over the next few difficult months when pressure on acute services, may make educational release difficult. If this becomes a consistent issue it is important that trainees discuss this with their Programme Directors. Any other additional work pressures as well as individual and personal issues should be discussed with the Programme Directors who will support you and offer advice as to how best to seek appropriate help.
Within the GP School, there are more trainees than ever before. There are also more trainers than any other Deanery, giving a blend of experience and enthusiasm for General Practice. The sixteen training programmes in the West Midlands have a superb cohort of Programme Directors and Associate Deans to support them (who are also happy to be contacted about concerns or issues).